Chronic Venous Insufficiency (CVI) is a condition affecting millions worldwide, primarily impacting the lower limbs. As a leading cause of varicose veins, swelling, and skin changes, accurate diagnosis is crucial for effective management. Duplex ultrasound scanning stands as the cornerstone imaging modality for CVI assessment. A key aspect that sonographers and specialists look for is the CVI reading obtained from the scan tool. But what does a high CVI reading on a scan tool usually indicate? This article, crafted by a seasoned auto repair expert turned content creator at vcdstool.com with a newfound passion for medical writing, will delve into the interpretation of these readings, ensuring you understand their significance in diagnosing and managing CVI.
Decoding CVI Readings: More Than Just Numbers
When we talk about a “high CVI reading,” we’re generally referring to findings during a duplex ultrasound that suggest significant venous reflux or incompetence. The scan tool, in this context, is the duplex ultrasound machine, a sophisticated device that uses sound waves to visualize blood flow within veins. A normal, healthy vein ensures unidirectional blood flow back to the heart, thanks to competent valves. However, in CVI, these valves become faulty, leading to retrograde blood flow or reflux. This reflux is what the scan tool detects and quantifies, giving us the “CVI reading.”
What Sonographers Need to Identify
For specialists treating CVI, the duplex ultrasound is more than just a scan; it’s a roadmap. The information gleaned from it dictates treatment strategies. Therefore, a comprehensive CVI duplex scan must answer critical questions:
- Deep Vein Status: Are the deep veins, the primary pathways for blood return from the legs, functioning correctly?
- Source of Reflux: Where is the reflux originating? Identifying the source is paramount for targeted treatment.
- Reflux Pathway: What is the route of the reflux? Which tributaries are affected, and how do they communicate?
- Pre-Catheter Assessment: If catheter-based interventions are considered, are there any obstructions or anatomical challenges that could hinder guide wire passage?
- Saphenous Vein Integrity: Is the saphenous vein, a key superficial vein, properly contained within its fascial envelope, a crucial detail for certain treatments?
The sonographer, the expert operating the scan tool, plays a pivotal role. They are not just technicians but skilled professionals with specialized training in venous hemodynamics and vascular duplex ultrasound. Their expertise ensures accurate data collection and interpretation, directly impacting patient care.
The Comprehensive CVI Examination Process
A high-quality CVI assessment involves more than just pointing the ultrasound probe. It begins with a thorough approach:
- Patient History: Understanding the patient’s symptoms, medical history, and risk factors.
- Visual Assessment: Observing the legs in a standing position under good lighting to identify varicose veins, skin changes, and areas of concern.
- Duplex Ultrasound Scan: The core of the examination, focusing on:
- Deep System: Assessing major deep veins like the femoral and popliteal veins.
- Superficial System: Examining superficial veins, including the great and small saphenous veins and their tributaries.
- Perforator Veins: Identifying incompetent perforator veins that connect superficial and deep systems.
- Extended Examination (If Necessary): Including iliac and ovarian veins when pelvic venous insufficiency is suspected.
This comprehensive approach ensures no critical venous segments are overlooked, and the root cause of CVI is accurately identified.
Interpreting High CVI Readings and Crafting a Report
The sonographer’s task culminates in a detailed graphical report for the specialist. This report is the primary communication tool, translating complex ultrasound findings into actionable information. A high CVI reading, visualized and quantified by the scan tool, is meticulously documented. The goal is to leave no questions unanswered regarding the patient’s venous hemodynamics and varicose vein distribution.
Time Allocation for Precision
While efficiency is important, rushing a CVI examination can compromise accuracy. Professional guidelines recommend a reasonable time allocation for these scans, acknowledging that complex cases, especially those involving recurrent varices or pelvic vein assessment, may require more time. Allocating adequate time ensures thoroughness and reduces the likelihood of overlooking subtle but significant findings that contribute to a high CVI reading.
Patient Preparation and Optimal Positioning
Vein distension is crucial for accurate assessment. Therefore, patient preparation plays a vital role:
- Avoid Stockings: Patients should avoid wearing compression stockings on the day of the exam.
- Warm Environment: Ensuring the patient and examination room are comfortably warm to promote vasodilation.
- Reverse Trendelenburg or Upright Position: Scanning in a reverse Trendelenburg position or with the patient standing maximizes hydrostatic pressure, distending the veins for better visualization and reflux detection.
- Fasting (If Pelvic Vein Assessment is Expected): Fasting for 6-8 hours minimizes bowel gas interference if ovarian and internal iliac veins need to be examined.
Proper patient positioning, often using a tilt-table, facilitates optimal venous distension and sonographer access, contributing to the accuracy of CVI readings.
Characteristics of Healthy vs. Unhealthy Veins: Identifying a High CVI Reading
Understanding the characteristics of normal veins is essential to identify abnormalities that contribute to a high CVI reading. Normal lower extremity veins should exhibit:
- Thin, Smooth Walls: Indicating healthy vessel structure.
- Complete Compressibility: Veins should easily compress under probe pressure, excluding thrombus.
- Spontaneity: Flow should be spontaneously observed, though this may be subtle in calf veins.
- Consistent Color Fill: Absence of color defects suggests unobstructed flow.
- Smooth Flow Contour: Laminar flow without disturbances.
- Phasicity: Respiratory variation in flow velocity, reflecting normal physiology.
- Augmentability: Prompt flow velocity increase with distal compression release.
- Competence: Unidirectional, cephalad flow maintained by competent valves.
- Non-Pulsatility: Minimal cardiac pulsatility in peripheral veins.
Deviations from these characteristics, particularly the absence of competence and the presence of reflux, are key indicators of a high CVI reading.
Figure 1: Competent Superficial Vein
Valves, Competence, and Incompetence: The Root of High CVI Readings
Venous valves are the gatekeepers of unidirectional flow in leg veins. Their failure is the primary culprit behind CVI and high CVI readings. These valves, typically bicuspid, prevent backflow of blood against gravity. In CVI, valve failure leads to venous reflux, venous hypertension, and the cascade of symptoms associated with the condition.
Valve failure can manifest in various reflux patterns, from minor “leaks” at the cusp tips to gross, spontaneous incompetence. Importantly, normal valves should withstand physiological pressures. Therefore, stress maneuvers during duplex scanning are crucial to provoke reflux and identify incompetence, especially in early CVI cases.
The pattern of superficial venous reflux is often “top-down.” Failure of proximal valves leads to dilation of downstream veins, increased pressure on subsequent valves, and a domino effect of valve incompetence extending down the leg. This cascade contributes to higher CVI readings as more extensive reflux is detected.
Provoking Reflux: Testing for Venous Incompetence
To accurately assess venous competence and detect reflux, sonographers employ various techniques to increase venous pressure and stress the valves:
- Valsalva Maneuver: Forced expiration against a closed airway to increase intrathoracic and intra-abdominal pressure.
- Simulated Valsalva: Applying abdominal pressure while the patient holds their breath.
- Manual Distal Augmentation: Squeezing the calf or thigh distally to propel blood centrally, followed by rapid release.
- Automated Cuff Augmentation: Using a pneumatic cuff for standardized distal compression and release.
- Calf Muscle Pump Activation: Plantar flexion to engage the calf muscle pump and assess valve function under physiological stress.
The Valsalva maneuver is particularly useful for assessing proximal veins like the common femoral vein. Distal augmentation is effective for evaluating veins below the saphenofemoral junction. The duration and strength of augmentation significantly impact reflux detection and quantification, directly influencing the CVI reading.
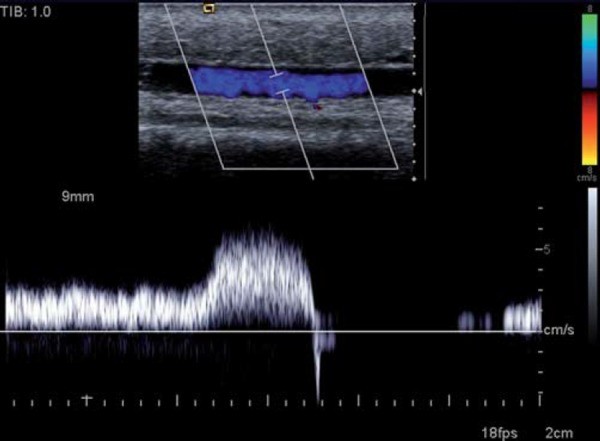
Figure 2: Refluxing Deep Vein
Figure 3: Variability of Reflux Response
Alt text: Spectral Doppler images demonstrating the effect of augmentation duration on reflux time in the popliteal vein, highlighting the variability of reflux response and the need for standardized techniques to ensure consistent CVI readings.
Defining Reflux: Setting the Diagnostic Threshold for High CVI Readings
Normal valve closure is rapid, with minimal retrograde flow during closure. The diagnostic threshold for reflux, indicative of a high CVI reading, is generally defined as retrograde flow exceeding 0.5 seconds. Some labs use a more stringent 1-second threshold. Superficial venous reflux often manifests as continuous flow lasting several seconds, easily exceeding both criteria.
While reflux time measurement is a practical diagnostic tool, more complex parameters like reflux waveform surface area and velocity have been explored. However, the anatomical variability of the venous system and the subjectivity of reflux elicitation make rigid hemodynamic criteria challenging to implement universally. The definition of reflux and the threshold for a “high CVI reading” often rely on accepted conventions and agreement between specialists and sonographers.
Figure 4: Refluxing Superficial Vein
Optimizing Duplex Imaging: System Settings for Accurate CVI Readings
The quality of the ultrasound system directly impacts the accuracy of CVI readings. While medium-level portable systems can suffice, dedicated vascular labs benefit from high-end scanners. Key system optimization strategies include:
- Transducer Selection: Medium to low-frequency linear transducers (5-8 MHz) for deep veins and high-frequency linear transducers (10-12 MHz) for superficial veins.
- Color Doppler as a Surveillance Tool: Utilizing color Doppler for efficient reflux detection and localization due to its rapid image acquisition, especially with modern systems featuring multiple beam formers and large color boxes.
- Spectral Doppler for Quantification: Employing spectral Doppler for accurate reflux time measurement, which color Doppler alone cannot provide.
- Doppler Angle Optimization: Maintaining a Doppler angle of ≤ 60° for both color and spectral Doppler to ensure accurate velocity measurements and reflux detection, especially in slow flow states.
- Optimized Doppler Settings: Using low scale and high gain for color Doppler and low scale and low wall filter for spectral Doppler to maximize Doppler shift display and waveform clarity.
Transverse scanning can be useful in some cases, but longitudinal views are generally preferred to maintain an optimal Doppler angle, particularly for subtle reflux detection.
Figure 5: Color Doppler Survey
Alt text: Color Doppler ultrasound images illustrating the use of large color boxes for efficient venous survey, showcasing the confluence of the profunda femoris vein and femoral vein (left) and femoral vein duplication (right), aiding in comprehensive CVI assessment.
Figure 6: Refluxing Flow Jets at Incompetent SFJs
Deep Vein Survey: Ruling Out Deep Venous Incompetence
A CVI scan includes a deep vein survey similar to a DVT scan but with added reflux assessment in the distal common femoral vein, femoral vein, and popliteal vein. While some labs may limit reflux testing to the femoral and popliteal veins due to common reflux in the common femoral vein even in normal subjects, comprehensive deep vein assessment is crucial. Reflux extending to the popliteal vein warrants calf vein evaluation as well.
Anatomical duplications, common in the popliteal (20%) and femoral veins (10%), necessitate testing of both duplicated vessels, as one may be incompetent while the other is competent, impacting the overall CVI reading.
Spectral Doppler waveforms in deep veins provide additional diagnostic clues. Absent respiratory phasicity in the common femoral vein waveform may indicate iliac vein obstruction. Pulsatile peripheral venous waveforms can suggest elevated central venous pressure, often associated with right heart failure.
Figure 7: Duplication of the Femoral Vein
Alt text: Duplex ultrasound images of a duplicated femoral vein during (left) and after (right) augmentation, revealing reflux in the more superficial of the two femoral veins, highlighting the importance of identifying and assessing venous duplications for accurate CVI readings.
Figure 8: Abnormal “Flat” Aphasic Femoral Vein Waveform
Figure 9: Pulsatile Venous Waveforms in POP Vein with CHF
Alt text: Spectral Doppler waveforms from the popliteal vein showing pulsatile flow in patients with congestive heart failure; competent (left) and incompetent (right) pulsatile popliteal vein, demonstrating how systemic conditions can influence venous waveforms and CVI readings.
Superficial Vein Anatomy: Navigating the Varicose Vein Maze
The superficial venous system exhibits significant anatomical variability. Key anatomical considerations include:
- Saphenofemoral Junction (SFJ) Location: Relatively constant at the groin crease.
- Saphenous Fascial Envelope: The great saphenous vein and its tributaries reside within a fascial envelope (“Saphenous eye”).
- Accessory Saphenous Veins: Anterior accessory saphenous vein (AASV) is common, typically superficial to the femoral vein, with the true GSV medial to it.
- Venous Duplications: Short-course duplications of GSV and SSV are common; full-length duplications are rare.
- Saphenopopliteal Junction (SPJ) Variability: Location varies significantly (medial, lateral, knee crease, absent, duplicated).
- Thigh Extension of SSV (TE SSV): SPJ may be absent, with SSV draining via TE SSV into other veins, including the vein of Giacomini connecting SSV and GSV.
- Intersaphenous Connections: GSV and SSV communicate via intersaphenous veins, especially in the calf, acting as potential reflux pathways.
Understanding these anatomical nuances is crucial for accurate mapping of reflux pathways and interpreting high CVI readings, especially in complex varicose vein patterns.
Figure 10: The Saphenous Fascial Envelope
Figure 11: Accessory Saphenous and Circumflex Veins of Thigh
Alt text: Duplex ultrasound image showing multiple superficial veins in the thigh, including the anterior accessory saphenous vein (AASV) superficial to the GSV, demonstrating the complexity of superficial venous anatomy relevant to CVI assessment and high CVI readings.
Figure 12: Superficial Veins of the Leg – Diagram
Common Patterns of Superficial Reflux: Understanding High CVI Readings
Most primary lower extremity varices stem from reflux at the SFJ or SPJ. Perforator incompetence can contribute to CVI or result from underlying CVI. Isolated primary perforator incompetence is less common. Pelvic venous incompetence is a significant CVI cause, especially in multiparous women, with refluxing pelvic veins connecting to lower extremity veins. Even with a competent SFJ, an incompetent GSV can be fed by the inferior epigastric vein. These diverse reflux patterns contribute to varying degrees of high CVI readings.
Figure 13: Patterns of Venous Reflux – Diagram
Alt text: Diagram illustrating common patterns of venous reflux in the lower extremity: junctional incompetence, isolated perforator incompetence, pelvic venous incompetence, and combined patterns, demonstrating the varied sources of reflux contributing to high CVI readings.
Figure 14: Competent SFJ with GSV Reflux Supplied by IEV
Simplifying the Examination: Strategies for Efficiency and Accuracy
CVI scanning can be complex, especially with extensive varices. Simplifying strategies include:
- Source-Path Approach: Identify the reflux source first, then trace the pathway.
- Overview Before Detail: Get a general overview of CVI extent before detailed tributary assessment.
- Color Doppler for Survey: Use color Doppler for efficient vein surveying and reflux screening.
- Vessel Size as a Clue: Superficial veins > 5 mm often reflux, but smaller veins can also be incompetent.
- Varicose Veins Invariably Reflux: No need to test clinically obvious varicose veins for reflux.
- Selective Testing of Tributaries: Focus testing on tributaries connected to incompetent vessels or with intercommunicating vessels.
- Note-Taking/Sketching: Maintain examination notes or sketches in complex cases to track examined segments.
These strategies streamline the examination, improve efficiency, and maintain accuracy in detecting reflux that leads to high CVI readings.
Figure 15: Determining the Path of Reflux
Figure 16: Duplex Sampling Sites – Diagram
Perforator Veins: Assessing Incompetence
A complete CVI exam includes searching for incompetent perforator veins. High-frequency transducers facilitate visualization of even normal perforators. Incompetent perforators are typically larger (> 3 mm). Thorough testing, especially over local varices, is crucial due to complex flow patterns. Location and diameter of incompetent perforators should be documented in the report, contributing to a comprehensive CVI reading.
Figure 17: Location and Nomenclature of Lower Extremity Perforators – Diagram
Recurrence: Investigating Post-Treatment Varices
Patients with recurrent varices require similar examination methods as initial presenters. Recurrence can arise from technical failures, neovascularization, disease progression, or perforator incompetence. Neovascularization at the SFJ, a network of tiny incompetent vessels, can be challenging to visualize but may be revealed by forceful Valsalva with color Doppler. Investigating recurrence is crucial for managing persistent symptoms and understanding why a patient might continue to have high CVI readings post-treatment.
Figure 18: Neovascularity at SFJ Ligation Site
Pelvic and Ovarian Veins: Considering Pelvic Venous Insufficiency
Pelvic venous incompetence, particularly of ovarian and internal iliac veins in women, can contribute to lower extremity varicose veins and recurrence. When pelvic venous insufficiency is suspected clinically or based on lower extremity findings, transabdominal pelvic vein assessment should be performed. This extended examination helps identify pelvic sources of reflux that can contribute to high CVI readings in the legs.
Reporting Results: Communicating High CVI Readings Effectively
The duplex scan report significantly impacts treatment decisions. A high-quality graphical report detailing superficial and deep veins, refluxing veins, varicose vein location, vessel sizes, anatomical variants, and other findings is crucial. Graphical reports are preferred over text reports for clarity and ease of interpretation by vascular specialists. These reports translate the “high CVI reading” into a comprehensive clinical picture.
Figure 19: Venous Duplex Reports – Examples
Figure 20: Screen Capture of Reporting PC
Alt text: Screenshot of a reporting PC setup with dual monitors, showing image review on one screen and report composition on the other, illustrating the workflow for efficient and detailed CVI report generation and communication of scan findings.
Frequently Asked Questions: Addressing Common Concerns About CVI Readings
- How many times should an incompetent vein be tested? Minimize retesting after reflux is established. Use color Doppler for survey and spectral Doppler for recording.
- Cannot find reflux source despite seeing incompetence? Always a source. Check for off-axis leaks, overlooked junctional reflux, neovascularization in recurrence, and pelvic sources.
- Patients with minor cosmetic veins? Scan later in the day when incompetence may worsen. Warm room. Ask patient to identify problem veins.
- CVI signs but no deep or superficial incompetence? Consider calf muscle pump deficiency, microvascular arterial disease, increased central venous pressure, popliteal vein compression syndrome, and patient factors like obesity and diabetes, particularly in certain populations.
Conclusion: The Significance of a High CVI Reading
Vascular specialists rely on high-quality duplex examinations to guide lower extremity venous interventions. A high CVI reading on a scan tool is a crucial indicator of venous incompetence, guiding diagnosis and treatment. Sonographers play a vital role in providing complete assessments and accurate reports. Effective CVI examinations, while detailed, can be time-efficient with strategic approaches. Understanding what a high CVI reading on a scan tool usually indicates empowers both clinicians and patients in the management of chronic venous insufficiency.
Acknowledgments
Grateful to Dr. Isabel Wright, Bridget Boyle, Mai Snelgrove, and Mr. David Ferrar for their manuscript review and constructive feedback.
References
(References from the original article should be listed here, maintaining the original numbering if possible, or re-numbered in a consistent format.)