Musculoskeletal conditions, ranging from degenerative diseases to traumatic injuries, present complex diagnostic challenges. Traditional methods often fall short in providing the accuracy and detail needed for effective treatment planning. However, the emergence of advanced diagnostic tools, akin to the precision of a Cat Mtp Scan Tool in automotive repair, is transforming musculoskeletal imaging. Integrated Single-Photon Emission Computed Tomography/Computed Tomography (SPECT/CT) is one such revolutionary technology, offering unparalleled insights into musculoskeletal pathology. This article explores the principles, techniques, and diverse applications of SPECT/CT, highlighting its role as a cutting-edge cat mtp scan tool for the human body.
1. Introduction: The Need for Precision in Musculoskeletal Imaging
The musculoskeletal system is susceptible to a wide array of conditions, including degenerative disorders, tumors (both benign and malignant), infections, inflammatory processes, metabolic diseases, and trauma. Bone scintigraphy, utilizing bisphosphonate radiopharmaceuticals, has long been a sensitive method for detecting functional and metabolic changes in bone, often preceding morphological changes visible on conventional imaging. This is because these agents are preferentially deposited at sites of altered bone turnover and remodeling, areas of increased osteoblastic activity. Whole-body scintigraphy offers a unique advantage by assessing the entire skeleton, unlike localized anatomical imaging techniques.
Planar bone scintigraphy (bone scan) with a 99mTc bisphosphonate agent is highly sensitive for detecting early functional bone derangements, indicative of osteoblastic remodeling. However, its specificity is limited, as various conditions can trigger such remodeling. Furthermore, planar bone scans lack the 3-dimensional depth perception crucial for precise localization, similar to the limitations of a 2D blueprint compared to a 3D model. Single-photon emission computed tomography (SPECT) adds this crucial 3D dimension, but it still lacks the detailed morphological information needed to pinpoint the cause of increased osteoblastic activity.
While side-by-side comparisons of SPECT and CT scans or plain radiographs can offer correlative information, localization remains approximate. This is where combined single-photon emission computed tomography/computed tomography (SPECT/CT) emerges as a superior solution. By seamlessly integrating the functional information from SPECT with the precise localization and morphological characterization of CT, SPECT/CT overcomes these limitations. This fusion of functional and anatomical imaging, much like a cat mtp scan tool providing both diagnostic codes and detailed system schematics, is increasingly recognized for its diagnostic value.
Early attempts at image fusion using software to co-register SPECT and CT information acquired separately faced challenges, particularly in the chest and abdomen, due to patient motion and organ movement. Even in skeletal imaging, factors like table curvature could affect spinal positioning, hindering accurate fusion. Clinical use of fusion software was often time-consuming and technically demanding.
The success of integrated Positron Emission Tomography (PET)/CT systems paved the way for commercial interest in SPECT/CT. Just as PET/CT enhanced PET imaging, SPECT/CT promised to significantly improve upon planar imaging and SPECT alone by increasing specificity and enabling accurate anatomical localization. This marked a new era of hybrid imaging, expanding the capabilities of nuclear medicine, and establishing SPECT/CT as an essential cat mtp scan tool equivalent for musculoskeletal diagnostics.
Early SPECT/CT systems, like the Hawk-Eye system, used low-dose CT primarily for attenuation correction in SPECT images and basic anatomical reference. However, rapid technological advancements have led to current SPECT/CT systems incorporating diagnostic-quality multi-slice CT technology. Algorithms for metal artifact reduction, crucial for evaluating joint prosthetics, and software like xSPECT Bone® further enhance image quality. The ability to determine Standardized Uptake Values (SUVs) on SPECT/CT images and new detector technologies like cadmium-zinc-telluride (CZT) continue to push the boundaries of this powerful diagnostic modality.
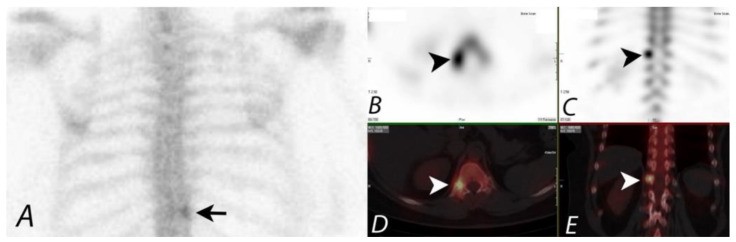
2. Oncologic Applications: Detecting and Characterizing Bone Metastases
Whole-body bone scintigraphy is a cornerstone in evaluating skeletal metastatic disease, a critical factor in cancer management and prognosis. While planar imaging can identify areas of concern, differentiating benign from malignant lesions can be challenging. SPECT improves sensitivity and accuracy, especially in the spine, but precise localization and characterization often require correlation with anatomical imaging. Similar to how a cat mtp scan tool can pinpoint the exact faulty component in a complex engine, SPECT/CT provides the definitive detail needed in oncology.
Studies consistently demonstrate that SPECT/CT significantly increases diagnostic specificity and viewer confidence compared to SPECT alone or side-by-side interpretation. In one study, SPECT/CT achieved a specific diagnosis in 100% of cases compared to 86% with SPECT and 64% with planar scintigraphy. SPECT/CT dramatically enhances the diagnostic value of bone scans in oncology, acting as a cat mtp scan tool to accurately identify and characterize bone lesions.
Multiple studies have confirmed the superiority of SPECT/CT in differentiating benign from malignant bone lesions. SPECT/CT correctly classified 85% of indeterminate scintigraphic bone lesions compared to only 36% with SPECT alone in one prospective study. Retrospective studies have shown SPECT/CT clarifying up to 92% of lesions indeterminate on SPECT. Furthermore, SPECT/CT has been shown to identify additional metastatic sites in a significant percentage of patients, highlighting its comprehensive diagnostic capability.
While low-dose CT protocols are often used in SPECT/CT, studies indicate no significant difference in lesion characterization compared to higher-dose diagnostic CT in this context. The potential of contrast-enhanced SPECT/CT is being explored, potentially streamlining diagnostic pathways for certain cancers.
3. Non-Oncologic Applications: Expanding Diagnostic Utility Beyond Cancer
The application of SPECT/CT extends beyond oncology, proving invaluable in evaluating benign musculoskeletal pathology. Similar to a versatile cat mtp scan tool used for diverse automotive issues, SPECT/CT addresses a wide spectrum of non-cancerous musculoskeletal conditions.
In a prospective study, SPECT/CT provided added clinical value in 89% of non-oncological patients with non-specific planar imaging findings. It reached a final diagnosis in 59% of patients, often eliminating the need for further imaging. Another study demonstrated SPECT/CT leading to revisions in diagnostic categories in a significant proportion of patients with extremity pain, reclassifying osteoarthritis as fractures or tumors, and osteomyelitis as osteoarthritis or soft tissue inflammation. This highlights SPECT/CT’s ability to refine diagnoses and guide appropriate management.
4. Evaluation of Spinal Pain: Pinpointing Pain Generators
Chronic spinal pain, often stemming from degenerative disease, is a prevalent clinical challenge. Identifying the precise pain generator is crucial for effective management. Anatomical imaging like radiography, CT, or MRI can reveal degenerative changes, but they often fail to pinpoint the exact pain source. Bone scintigraphy with SPECT or SPECT/CT, acting like a cat mtp scan tool for the spine, excels at localizing metabolically active sites of disease.
99mTc-MDP bone SPECT has proven predictive of active facet joint disease. Studies have shown SPECT identifying lesions not detected by planar imaging, and SPECT lesions frequently correlating with abnormalities seen on CT. SPECT and SPECT/CT can guide therapeutic interventions by differentiating facet joint arthropathy from costovertebral joint osteoarthritis, facilitating targeted facet joint injections.
SPECT/CT can also be valuable in patients with osteoporotic vertebral collapse and chronic back pain, helping determine if pain originates from facet joints rather than the fracture itself. While MRI remains the primary imaging modality for back pain due to its soft tissue sensitivity and lack of radiation, SPECT/CT is a valuable problem-solving tool, especially when MRI is contraindicated.
5. Postoperative Spine Assessment: Diagnosing Failed Back Syndrome
Persistent or recurrent pain after spinal surgery, known as failed back syndrome, is a significant clinical problem. Accurately identifying patients who would benefit from re-intervention is critical, as outcomes after revision surgery are often less favorable. Conventional imaging modalities like radiography, MRI, or CT can assess hardware position and bony fusion, but MRI is limited by metal artifacts, and CT has limited sensitivity for evolving non-union. Bone scintigraphy with SPECT/CT offers a valuable solution, acting as a cat mtp scan tool to diagnose post-surgical complications.
SPECT/CT is particularly useful in evaluating pseudarthrosis or non-union, a major cause of failed back syndrome. While physiological remodeling after surgery can cause non-specific uptake on bone scans, persistent increased activity beyond a year post-surgery suggests pseudarthrosis. SPECT/CT’s high sensitivity and specificity, combining functional and anatomical information, make it superior to SPECT alone, which has a high false-positive rate. SPECT/CT is recommended as an effective modality for evaluating failed back syndrome and other post-surgical complications, including hardware failure.
6. Hip Pain Evaluation: Diagnosing Impingement and Prosthetic Complications
SPECT/CT is expanding its role in hip pain evaluation, especially when MRI is contraindicated or inconclusive. It offers whole-body skeletal assessment and detailed regional evaluation, making it a comprehensive tool, much like a multifaceted cat mtp scan tool. Indications include impingement, stress fractures, avascular necrosis, heterotopic ossification, joint replacement assessment, and unexplained hip pain.
SPECT/CT aids in diagnosing conditions like femoral acetabular impingement syndrome (FAI), often misattributed to degenerative disease. It can detect uptake patterns suggestive of cam or pincer impingement. In patients on bisphosphonates, SPECT/CT readily identifies subtle stress fractures, often missed on anatomical imaging.
For total hip arthroplasty, SPECT/CT is valuable in evaluating persistent pain, differentiating between aseptic loosening and infection, crucial for determining the appropriate revision surgery approach. Three-phase bone scans with SPECT/CT improve specificity in diagnosing loosening and infection, with the CT component providing additional information like fluid collections suggestive of infection. SPECT/CT is particularly useful for evaluating heterotopic ossification after hip replacement, guiding timely surgical intervention.
7. Knee Pain Management: Assessing Prosthetic and Intra-articular Issues
MRI is often the primary imaging modality for knee pain, but SPECT/CT excels in situations with metallic implants or when MRI is contraindicated. SPECT/CT, akin to a specialized cat mtp scan tool for the knee, is superior for evaluating cortical bone and in the presence of metal artifacts.
SPECT/CT, combined with arthrography, can assess soft tissue structures like cartilage, menisci, and ligaments. It’s useful for detecting meniscal tears, ligament injuries, and intra-articular loose bodies. SPECT/CT also aids in evaluating tumors around the knee, osteochondral defects, ligament repair sites, and pain after total knee arthroplasty.
SPECT/CT is proposed as a second-line imaging modality after MRI for painful knee prostheses. It increases specificity by accurately localizing uptake, distinguishing granulomatous processes from physiological uptake. SPECT/CT significantly impacts patient management in up to 85% of cases, highlighting its clinical utility in knee pain assessment.
8. Extremity SPECT/CT: Enhancing Diagnosis in Complex Joints
The intricate anatomy of small joints in the wrist, ankle, and foot makes planar and SPECT imaging challenging. SPECT/CT provides crucial anatomical landmarks, allowing for accurate localization of tracer activity. This advantage helps differentiate degenerative changes from tumors or occult trauma, acting as a precise cat mtp scan tool for extremities.
Studies show SPECT/CT providing additional diagnostic information in 81% of patients with ankle/foot pain, altering management plans in up to 62%. SPECT/CT interpretation has changed management approaches in a significant percentage of patients with osteochondral defects of the talus. It’s also valuable in assessing post-joint fusion, tarsal coalition, post-operative infection, Achilles tendonitis, plantar fasciitis, stress fractures, and painful accessory bone syndromes.
SPECT/CT is particularly useful in post-surgical foot and ankle assessments, where metallic artifacts limit CT and MRI. It helps diagnose non-union, mal-union, loosening, or degenerative changes after joint fusion. For tendinitis and similar pathologies, SPECT/CT provides valuable information for better patient management.
9. Infection and Inflammation: Distinguishing Osteomyelitis
SPECT/CT significantly improves the diagnosis of skeletal infection and inflammation due to enhanced tissue contrast and precise anatomical localization. Distinguishing osteomyelitis from other bone pathologies is diagnostically challenging. While conventional radiography and CT can reveal advanced osteomyelitis, early stages are often missed. MRI is often the first advanced imaging method, but it’s limited by hardware, metal artifacts, and inability to use contrast in some patients. SPECT/CT offers a robust alternative, acting as a sensitive cat mtp scan tool for infection.
Three-phase bisphosphonate bone scans, enhanced by SPECT/CT, are valuable for identifying osteomyelitis. SPECT/CT helps differentiate various causes of positive bone scans by identifying specific bone morphology at the uptake site. WBC scans, labeled with 99mTc HMPAO or 111In oxine, combined with SPECT/CT, further improve the distinction between soft tissue and bone infection. WBC SPECT/CT can be used with Tc-99m bisphosphonate SPECT/CT for added confirmation of osseous remodeling.
SPECT/CT with labeled WBCs and Ga-67 scans improves the distinction between soft tissue and bone uptake, defining the extent of abnormality and enhancing diagnostic certainty. In spinal osteomyelitis, comparing WBC scans with 99mTc sulfur colloid scans, aided by SPECT/CT’s anatomical precision, helps differentiate infection from normal marrow uptake. SPECT/CT is critical for detailed definition of uptake sites in skull base osteomyelitis, often used with 99mTc bisphosphonate and Ga-67 scans for accurate diagnosis and differentiation of active infection from post-infectious remodeling.
10. Extraosseous Tracer Uptake: Unveiling Soft Tissue Pathology
Extraosseous uptake of 99mTc-MDP on bone scans can be caused by various non-osseous processes, including neoplastic, inflammatory, and traumatic conditions. SPECT/CT improves diagnostic interpretation by accurately localizing radiotracer accumulation in soft tissues, acting as a cat mtp scan tool to investigate these incidental findings.
SPECT/CT is particularly useful in evaluating heterotopic ossification, accurately localizing activity within soft tissues and differentiating it from adjacent osseous structures. It can also distinguish heterotopic ossification from clinically suspected osteomyelitis. Understanding the mechanisms of radiopharmaceutical uptake, combined with SPECT/CT’s precision, is crucial for determining the underlying cause of extraosseous activity.
11. Frostbite Assessment: Guiding Amputation and Reperfusion Strategies
In frostbite injuries, scintigraphic perfusion imaging with SPECT/CT plays a critical role in determining tissue devascularization, guiding amputation planning and reperfusion attempts. Early perfusion assessment is crucial, and SPECT/CT obtained during the blood pool phase accurately defines tissue perfusion relative to anatomical landmarks, acting as a vital cat mtp scan tool in managing frostbite.
SPECT/CT helps determine the level of soft-tissue non-perfusion, facilitating amputation at a level covered by well-perfused tissue. It also assesses the success of reperfusion attempts. Patterns of uptake on bone scan phases correlate with clinical management, ranging from hyper-perfusion in minor injuries to absent uptake in severe cases requiring amputation.
12. Conclusions: Embracing SPECT/CT for Enhanced Musculoskeletal Care
SPECT/CT is a transformative hybrid imaging modality, combining functional and anatomical information to enhance diagnostic accuracy and confidence in musculoskeletal imaging. Like a sophisticated cat mtp scan tool revolutionizing automotive diagnostics, SPECT/CT is revolutionizing musculoskeletal diagnostics, leading to significant impacts on patient management and outcomes. The growing evidence base supports its application in both oncologic and benign musculoskeletal conditions. Despite the use of ionizing radiation, the improved specificity, accurate localization, and reduced equivocal interpretations justify the increased adoption of SPECT/CT in clinical practice, ultimately improving patient care in musculoskeletal disorders.
Author Contributions
Conceptualization, R.K.J.B. and B.R.K.; methodology, R.K.J.B., B.R.K., K.A.M.; formal analysis, R.K.J.B., B.R.K., K.A.M., N.M.D., R.A.-D., G.C.F.; investigation, R.K.J.B., B.R.K., K.A.M., N.M.D., R.A.-D., G.C.F.; resources, R.K.J.B., K.A.M.; data curation, B.R.K.; writing—original draft preparation, B.R.K., K.A.M.; writing—review and editing, R.K.J.B., B.R.K., K.A.M., N.M.D., R.A.-D., G.C.F.; visualization, R.K.J.B., B.R.K., K.A.M., N.M.D., R.A.-D., G.C.F.; supervision, R.K.J.B.; project administration, B.R.K.; funding acquisition: not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This review article did not receive any external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
Richard K. J. Brown is on the Medical Advisory Board of Covera Health. However, the content of this paper is not related and there are no relevant conflicts of interest for any of the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.