Accurate diagnosis of middle ear cholesteatoma is crucial for effective treatment and preventing complications. Both Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) are essential diagnostic tools, providing detailed insights into the presence, extent, and characteristics of cholesteatoma. This article focuses on the clinically relevant imaging findings of middle ear cholesteatoma using CT and MRI, highlighting their individual strengths in diagnosis.
CT Scan Findings for Cholesteatoma
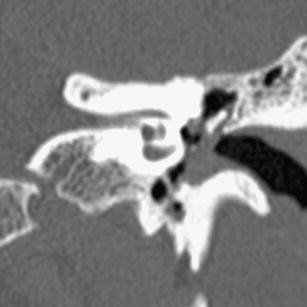
CT scans are highly effective in visualizing bony structures, making them excellent for identifying the erosive nature of cholesteatoma in the middle ear.
Typical CT Features of Cholesteatoma
On CT images, cholesteatomas typically appear as soft tissue masses. Key indicators include:
- Lobulated soft tissue mass: Visible adjacent to the ossicular chain, indicating potential cholesteatoma presence.
- Scutum erosion: CT scans can clearly demonstrate erosion of the scutum, a common finding in cholesteatoma cases, signaling bone destruction.
Key Features to Evaluate on CT for Middle Ear Cholesteatoma
When interpreting CT scans for cholesteatoma, specific anatomical features should be carefully assessed:
- Ossicle Erosion and Displacement: CT scans can reveal damage to the ossicles (malleus, incus, stapes) and any displacement due to cholesteatoma growth.
- Tegmen Tympani and Lateral Semicircular Canal Bony Cover: Assess the integrity of the bony cover of the tegmen tympani (roof of the middle ear) and the lateral semicircular canal, as erosion in these areas can indicate cholesteatoma extension.
- Facial Nerve Canal Walls: Evaluate the bony walls of the tympanic segment and anterior genu of the facial nerve canal for any signs of erosion or involvement.
- Sinus Tympani Extension: Check for cholesteatoma extension towards the sinus tympani, which is associated with a higher risk of post-surgical recurrence.
- Oval Window Niche Involvement: Determine if the cholesteatoma involves the oval window niche, which can impact surgical planning.
MRI Findings for Cholesteatoma
MRI excels in soft tissue differentiation and is particularly valuable in characterizing cholesteatoma tissue and distinguishing it from other middle ear pathologies.
Typical MRI Features of Cholesteatoma
MRI characteristics of cholesteatoma include:
- Hyperintense signal on Diffusion-Weighted MRI (DWI): Cholesteatomas show a bright, hyper-intense signal on B-1,000 DWI images, a key feature for identification.
- Hypointense signal on ADC map: Correspondingly, cholesteatomas exhibit a hypo-intense signal on the Apparent Diffusion Coefficient (ADC) map, confirming restricted diffusion.
- Lack of Enhancement on Post-Gadolinium T1-weighted sequences: Cholesteatomas typically do not enhance after gadolinium contrast administration, helping to differentiate them from inflammatory tissue.
Cholesteatomas also present with moderate intensity on T2-weighted images, which is lower than the high signal intensity seen in middle ear inflammation.
Clinical Applications of CT and MRI in Cholesteatoma Diagnosis
The choice between CT and MRI, or their combined use, depends on the clinical scenario and the stage of cholesteatoma management.
CT as Primary Imaging Tool: In cases with clear clinical and otoscopic suspicion of cholesteatoma, CT is often the primary imaging technique before initial surgery. CT effectively demonstrates ossicular and epitympanic erosion, tegmen integrity, and the status of the facial nerve and lateral semicircular canal.
MRI for Complex and Post-Operative Cases: MRI becomes essential when infection, inflammation, or complications like labyrinthine fistula are suspected. MRI can differentiate cholesteatoma from inflammation and assess the membranous labyrinth. Diffusion-weighted MRI is particularly useful as a screening tool to exclude cholesteatoma, especially non-echo planar DWI sequences which are preferred for accuracy.
MRI for Second-Look Surgeries: In revision surgeries, CT is limited in distinguishing soft tissues within the surgical cavity. MRI, especially diffusion-weighted imaging, is superior for detecting residual or recurrent cholesteatoma. Non-EP DWI sequences alone offer high sensitivity and specificity, comparable to combining DWI with delayed post-gadolinium T1-weighted sequences, making it a valuable tool for pre-second-look evaluations.
Conclusion
Both CT scans and MRI are indispensable diagnostic tools in the evaluation of middle ear cholesteatoma. CT is excellent for assessing bony erosion and anatomical detail, particularly in primary diagnosis and pre-operative planning. MRI, especially diffusion-weighted sequences, plays a critical role in differentiating cholesteatoma from inflammation, assessing complications, and detecting residual or recurrent disease, particularly in post-operative settings and revision surgeries. The strategic use of these diagnostic tools ensures optimal management and improved outcomes for patients with middle ear cholesteatoma.